
Roy A. Rothman, DPM, PA
Podiatric Medicine and SurgeonFoot & Ankle Specialist



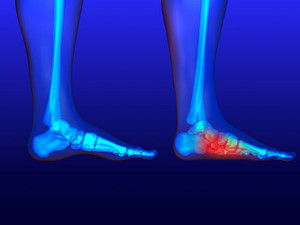
A broken foot occurs when one or more of the bones in the foot are fractured, often due to trauma, such as a fall, car accident, or sports injury. Symptoms typically include intense pain, swelling, bruising, and difficulty walking or bearing weight. The severity of the fracture, its location, and the treatment approach all influence healing time. Generally, a simple fracture can take six to eight weeks to heal, while more complex fractures may require several months, especially if surgery is needed. During the healing process, immobilization with a cast or boot is usually prescribed, and in some cases, crutches are provided to avoid putting weight on the foot. If you have broken your foot, it is suggested that you schedule an appointment with a podiatrist and follow their instructions to ensure proper healing and avoid complications.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Roy Rothman, DPM from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in DeBary, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
One out of ten broken bones is reported to be in the feet. When an object crushes, bends, or stretches the bone beyond acceptable ranges, bones break. A break in the foot is either a fracture or a straight break.
The location of any break can tell you how the break happened. Toes, for instance, break typically as a result of something being kicked hard and with great force. Heel breaks almost always are a result of an improper landing from a tall height. Twists or sprains are the other two frequent occurrences. As with all usual breaks, they result from unexpected accident or sudden injury. As with stress fractures, breaks form as a process over time from repeated stress on already present cracks. Runners, dancers, and gymnasts are the usual athletes who receive this type of break. Stress fractures result from incredible pressure on the feet. It is no surprise these athletes bear the majority of reported fractures.
Pain, swelling, bruising, and redness are all indicative of the typical symptoms from a broken foot. Severe pain—to the point of not being able to walk—usually depends on the location of the break in the foot. Toes are on the lower scale of pain threshold, but heels are high, as are a few other particular bones. As the severity of the broken foot increases, symptoms like blueness, numbness, misshaping of the foot, cuts, or deformities will become apparent. These symptoms indicate the need to see a medical professional with access to an x-ray facility.
Prior to seeing a specialist, precautions should be taken to reduce pain and swelling. Elevate and stabilize the foot, and refrain from moving it. Immobilization of the foot is the next priority, so creating a homemade splint is acceptable. Keep in mind that while creating a splint, any increase of pain or cutting off blood circulation means that the splint should be removed immediately. Use ice to decrease swelling and relieve pain symptoms.
When dealing with a medical center, the patient should note that the treatment can vary. The treatment will depend on the severity of the fracture and the cause of the break. Crutches, splits, or casts are common treatments while surgery has been known to be used in more severe cases in order to repair the break in the bones.

Running shoes and walking shoes are designed with distinct features tailored to their respective activities. Running shoes are built to handle the higher impact forces of running, featuring more cushioning in the heel to absorb shock and provide support during each stride. They often have a more pronounced heel-to-toe drop, which promotes a forward motion. In contrast, walking shoes are designed for lower impact and typically have a flatter sole, offering even cushioning and greater flexibility. The emphasis in walking shoes is on stability and comfort for the repetitive heel-to-toe motion of walking. Additionally, walking shoes usually have a more rigid midsole to support the arch and enhance stability. Choosing the appropriate shoe based on your activity helps prevent injury and ensures better performance and comfort. If you have endured a foot or ankle injury from wearing the wrong type of shoes, it is suggested that you consult a podiatrist who can treat various foot conditions, and guide you on which shoes to buy for your desired activity.
For more information about walking shoes versus running shoes, consult with Roy Rothman, DPM from Florida. Our doctor can measure your feet to determine what your needs are and help you find an appropriate pair of footwear.
Foot Health: The Differences between Walking & Running Shoes
There are great ways to stay in shape: running and walking are two great exercises to a healthy lifestyle. It is important to know that running shoes and walking shoes are not interchangeable. There is a key difference on how the feet hit the ground when someone is running or walking. This is why one should be aware that a shoe is designed differently for each activity.
You may be asking yourself what the real differences are between walking and running shoes and the answers may shock you.
Differences
Walking doesn’t involve as much stress or impact on the feet as running does. However, this doesn’t mean that you should be any less prepared. When you’re walking, you land on your heels and have your foot roll forward. This rolling motion requires additional support to the feet.
Flexibility – Walking shoes are designed to have soft, flexible soles. This allows the walker to push off easily with each step.
If you have any questions, please feel free to contact our office located in DeBary, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Although walking shoes and running shoes look similar, they have characteristics that make them different from each other. Runners should avoid running in walking shoes and vice versa. It is very important that you wear the proper footwear for the activity you are going to partake in, for you to avoid injury.
If you are looking to buy a new pair of running shoes, there are certain things you should look out for. One of the main components that makes up a good running shoe is flexibility. You should be able to bend and flex the forefoot of the shoe that you are purchasing. If you can bend the entire shoe in half with ease, this is a sign that the shoe does not have enough structure for your feet. Another feature you should look for is a low heel. Certain running shoes have a low heel to support runners who land on the ball of their feet. Lastly, you should look for the fit of the running shoe. You should visit the best running shoe store in your area to have your feet properly sized for the shoes in the store. Usually, the staff will be able to help recommend the best type of running shoe for your needs.
When you are walking, the body’s weight is evenly distributed on the foot. This influences the design of shoes made for walking. If you are looking to buy a pair of walking shoes, there are different features you should look for to determine which pair of shoes is best for you. Walking shoes should be flexible through the ball of the foot to allow for a greater range of motion through the roll of the forefoot. These shoes also should have greater arch support for the foot. If you plan on walking long distances or on hard surfaces, it is best that you wear shoes that have cushioning.
When trying on a new pair of shoes, the heel should fit snugly without slip. You should shop for shoes after a long walk, since your feet tend to swell throughout the day. Many people have one foot that is a different size than the other, so it is best that you have both feet measured when looking for your true size. You should also beware that sizes vary depending on the shoe brand. A certain size in one brand may be a different size in a different brand. Lastly, you should always walk around in shoes that you plan on buying. This will help you determine whether the shoes are comfortable and if they fit well on your feet.
Always look for good shoe construction when shopping for new sneakers. The upper part of the shoe should allow for adjustment through laces or straps. If you need help with shoe sizing or if you need custom orthotics for your feet, you should make an appointment with your podiatrist for assistance. He or she will be more than happy to help you with your shoe sizing needs.

Plantar fasciitis is a common cause of heel pain, primarily resulting from inflammation of the plantar fascia, the thick band of tissue running along the bottom of the foot. Common causes can include excessive stress from high-impact activities, prolonged standing, wearing unsupportive footwear, or being overweight. Symptoms typically include a sharp, stabbing pain in the heel, especially noticeable with the first steps in the morning or after prolonged periods of rest. Treatment focuses on reducing inflammation and relieving pain. Effective stretches include the calf stretch, where you press against a wall with one leg forward and the other extended back. Another is the plantar fascia stretch, where you pull your toes toward your shin while seated. Wearing supportive shoes or custom orthotics, in addition to performing these stretches, can provide significant relief. If you are experiencing symptoms of plantar fasciitis, it is suggested you schedule an appointment with a podiatrist for expert care to effectively manage your condition and improve your foot health.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Roy Rothman, DPM from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in DeBary, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Flat feet, or pes planus, come in two main types, which are flexible and rigid. Flexible flat feet show arches that flatten when standing but are visible when sitting, while rigid flat feet have no arch even when sitting. Symptoms often include foot pain, swelling, and difficulty walking or standing for long periods. Risk factors include genetic predisposition, obesity, and certain medical conditions like arthritis. To alleviate discomfort, specific stretches can be helpful. Stretching the Achilles tendon and calf muscles can relieve tension and improve foot flexibility. Foot exercises, such as toe curls and arch lifts, strengthen the muscles supporting the arch. If you have flat feet, it is strongly suggested that you are under the care of a podiatrist who can offer effective relief solutions.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Roy Rothman, DPM from Florida. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in DeBary, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flatfoot is a condition that occurs when the arches on the foot are flattened, which allows the soles of the feet to touch the floor. Flatfoot is a common condition and it is usually painless.
Throughout childhood, most people begin to develop arches in their feet, however, some do not. Those who do not develop arches are left with flatfoot. The pain associated with flat feet is usually at its worse when engaging in activity. Another symptom that may occur with those who have this condition is swelling along the inside of the ankle.
It is also possible to have flexible flatfoot. Flexible flatfoot occurs when the arch is visible while sitting or standing on the tiptoes, but it disappears when standing. People who have flexible flatfoot are often children and most outgrow it without any problems.
There are some risk factors that may make you more likely to develop flatfoot. Those who have diabetes and rheumatoid arthritis have an increased risk of flatfoot development. Other factors include aging and obesity.
Diagnosis for flat feet is usually done by a series of tests by your podiatrist. Your podiatrist will typically try an x-ray, CT scan, ultrasound, or MRI on the feet. Treatment is usually not necessary for flat foot unless it causes pain. However, therapy is often used for those who experience pain in their flat feet. Some other suggested treatment options are arch supports, stretching exercises, and supportive shoes.

Preventing falls both at work and in the home is vital for safety and well-being. In the workplace, maintaining a clean, clutter-free environment and ensuring that all walkways are well-lit can significantly reduce fall risks. Employees should be encouraged to use proper footwear with slip-resistant soles and to secure any loose cables or cords. At home, keeping floors tidy and free from obstacles is essential. Use non-slip mats in bathrooms and secure rugs to prevent slipping. Ensure adequate lighting in hallways and staircases to improve visibility. Installing handrails on stairs and in bathrooms can provide additional support. Additionally, regularly checking and repairing any worn or uneven flooring can also help prevent accidents. Various foot and ankle injuries can happen from falling. If this applies to you, it is suggested that you visit a podiatrist who can effectively treat these types of ailments, and guide you on additional fall prevention techniques.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Roy Rothman, DPM from Florida. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in DeBary, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.